Personalised medicine
In collaboration with its partners the National Institute for Health Development is carrying out a project called ‘Implementation of Personalised Medicine in Estonia’ (2019–2023) for setting up readiness to use genetic data on a wider basis in the work of physicians and nurses across the country.
What is personalised medicine?
Personalised medicine means an approach for finding an individualised prevention or treatment plan for each person by analysing the health data of the relevant person and their close family members along with data on their lifestyle and surroundings.
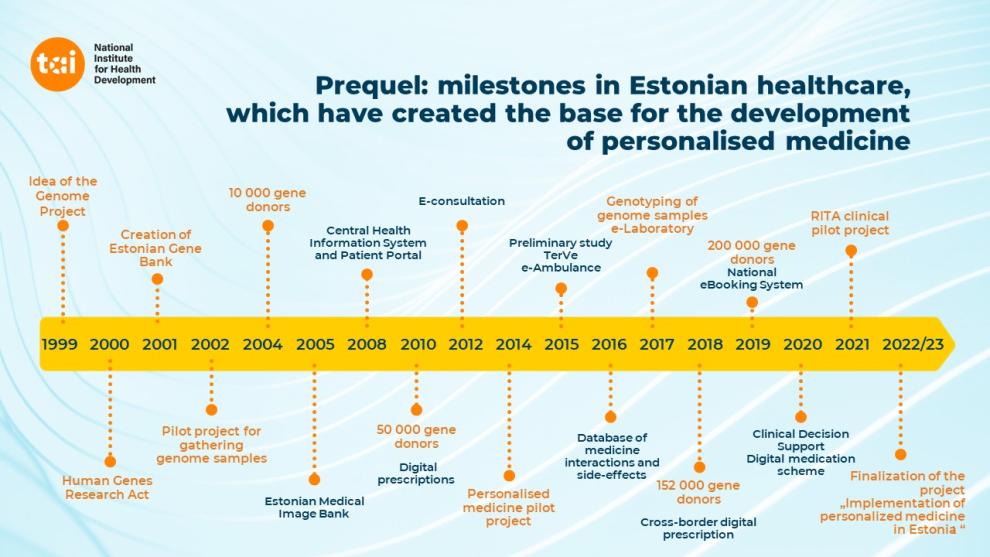
The development of e-Healthcare in Estonia has paved the way for personalised medicine
The Estonian Biobank has established a population-based biobank of Estonia with a current cohort size of more than 200,000 individuals (genotyped with genome-wide arrays), reflecting the age, sex and geographical distribution of the adult Estonian population. Each person in Estonia that has visited a doctor has an online e-Health record that can be tracked. Identified by the electronic ID-card, the health information is kept secure and at the same time accessible to authorised individuals.
Thus, Estonia has set up a system where health data are gathered into a single health information system and we have knowledge of genome data of nearly 20% of the country’s adult population. This creates a unique opportunity to apply personalised medicine in a way whereby genetic information added to health data allows making better prevention and treatment decisions.
Project actions
The implementation of the personalised medicine project helps to take into wider use one part of health data in personalised medicine – genetic data. The preconditions necessary for taking them into use will be created by the middle of 2023.
The first services planned to incorporate genetic data on a wider basis are the prevention and early detection of breast cancer and personal recommendations for medicinal products.
1. The project focuses on establishing an IT infrastructure
For genetic information to make its way to the healthcare professional’s desk it is necessary to develop:
- Consent Management System
- Genetic data Information System
- Monitoring and management platform for genetic risk models
- Computation Environment for Personalised Medicine where in the course of the project a capability is created to calculate:
- the genetic risk of cardiovascular diseases
- the genetic risk of breast cancer
- pharmacogenetic risks (for making recommendations when determining the active substance of medicinal products)
- Health and Treatment Recommendation System
2. Creating a legal framework and ensuring compliance with quality requirements
- We will create a legal framework for providing personalised medicine services
- We will create a system for ensuring service providers’ compliance with quality requirements
3. Training healthcare professionals
We will train health care professionals for taking genetic data into wider use.
4. Informing the public
We will provide people with information about personalised medicine services.
Project participants and their roles
The project is carried out by the National Institute for Health Development in collaboration with the University of Tartu, the Health and Welfare Information Systems Centre, the Estonian Health Insurance Fund and the Ministry of Social Affairs.
National Institute for Health Development
- Project management
- Heading the development of a quality management system
- Organisation and coordination of training courses
- Communication
Health and Welfare Information Systems Centre
- Improvement of the Health Information System, interfaces
- Improvement of the Patient Portal
- Integration of the Consent Management System
- Development of the Health and Treatment Recommendation System
- Hosting and administration of solution parts
University of Tartu
- Creation of software and applications:
– Genetic Data Information System
– Monitoring and management platform for genetic risk models
– Computation Environment for Personalised Medicine
- Development of and carrying out training courses
Estonian Health Insurance Fund
- Development of the Decision Support System
- Digital prescription management
Ministry of Social Affairs
- Development of the legal framework
The project ‘Implementation of Personalised Medicine in Estonia’ is carried out with the support of the European Regional Development Fund.
Related projects
An important input into applying personalised medicine is provided by clinical pilot projects (RITA projects) lead by the Tartu University Hospital. From 2017 to 2021 two clinical pilot projects were carried out:
- personal prevention and early detection of breast cancer
- prevention of cardiovascular diseases, statin treatment, ascertainment and application of personal indications.
The pilot projects carried out a research which served the aim of finding out how to use genetic data in personalised disease-preventing health services, and developing a service process. The research results are set out in the final report.
Framework documents
The application of personalised medicine in Estonia is based on the following documents:
- e-Health strategy which in one aspect focuses on persons and personalised medicine
- Estonia’s National Health Plan 2020–2030